Research & Outcomes
Patient Outcomes Study Results at Ashley
Ashley Addiction Treatment, established in 1983, has helped over 65,000 people with substance use disorders. We continue to serve our patients and the industry by being at the forefront of SUD treatment, driven by a vision of evidence-based, inclusive, and personalized care. This report highlights the research team’s efforts over the past four years in improving treatment outcomes, supported by collaborations with Johns Hopkins faculty.
What We Measured
How We Measured
Trac9 is a data driven tool for assessing and monitoring patient outcomes in addiction treatment. This
approach uses a battery of standardized assessments that collect patient reported mental health progress with a focus on risk and resilience factors.
The system has two primary uses:
1) empowering clinicians with real-time, visual charts of
patient progress, allowing them to tailor treatments and intervene
promptly, and
2) allowing the research department to gather more
granular data to identify factors linked to long-term success,
guiding our service optimization.
Biometrics
What it is: We utilize daily activity wearables to measure momentary health metrics related to sleep and cardiovascular health so that we can better understand how factors of physiological health are related to treatment outcomes.
How it works: In 2022, patients enrolled in residential and extended care treatment were offered activity wearables worn for the duration of their stay.
Why its important: Addiction treatment often lacks objective measures to track a patient’s recovery progress. However, our program uniquely combines self-reported data with physiological monitoring, offering a comprehensive picture of a patient’s health and well-being throughout their treatment journey.
Wearable Worn Throughout Residential Treatment & Extended Care
INTAKE
Collects foundational information
TREATMENT PROGRESS
Assesses risk and resilience factors
Weekly Survey’s (Admissions + 1X/ week)
DISCHARGE
Measures patient satisfaction
POST DISCHARGE
Tracks relapse, mood, and recovery resources
Monthly Survey’s (12 surveys – 1x/ month for 12 months)
Why We Measure
Addiction treatment should prioritize personalized care, informed decision-making, and quality of life. We utilize a unique combination of patient-reported outcomes, objective biometric data and academic research to unlock personalized treatment pathways and identify new therapeutic avenues to ensure the best possible outcomes.
Academic Studies
What it is: We deploy observational studies and clinical trials that delve into key factors contributing to recovery – sleep, chronic pain, withdrawal, craving, and emotion. These investigations illuminate the intricacies and effectiveness of various treatment modalities, both established and novel, while uncovering potential subgroup patterns during the recovery journey.
How it works: Through established collaborations with faculty from Johns Hopkins and academic investigators under IRB regulations, Ashley becomes a research site where project coordinators screen and enroll eligible and willing patients.
Why its important: From these studies, Ashley receives valuable firsthand insights into novel evidence-based interventions which improve overall treatment programming.
Who We Measure
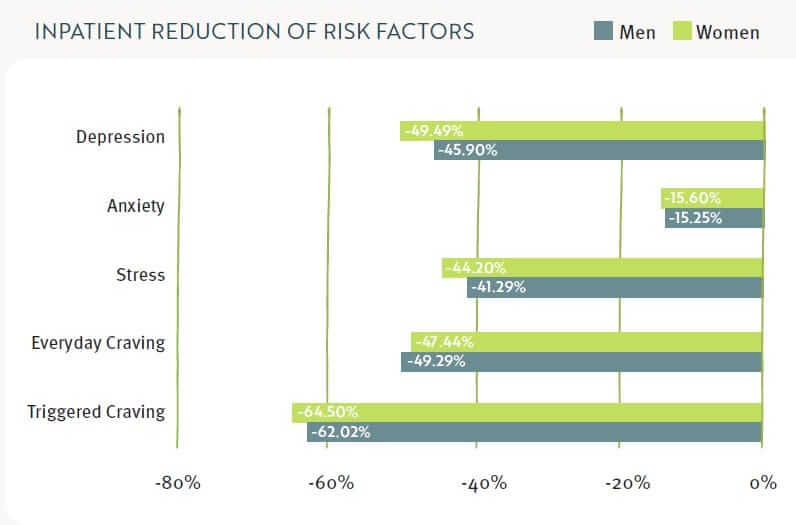
Our inpatient treatment program demonstrates a significant positive effect on known risk factors
for recovery in patients with substance use disorders. Notably, depression and craving showed the
greatest improvement. However, the changes in anxiety symptoms were relatively modest, averaging
around 15%.
Anxiety symptoms may improve more slowly than other factors, and these results highlight the
importance of monitoring these symptoms longer-term and the need for therapeutic tactics
which target symptoms of anxiety within our existing treatment model.
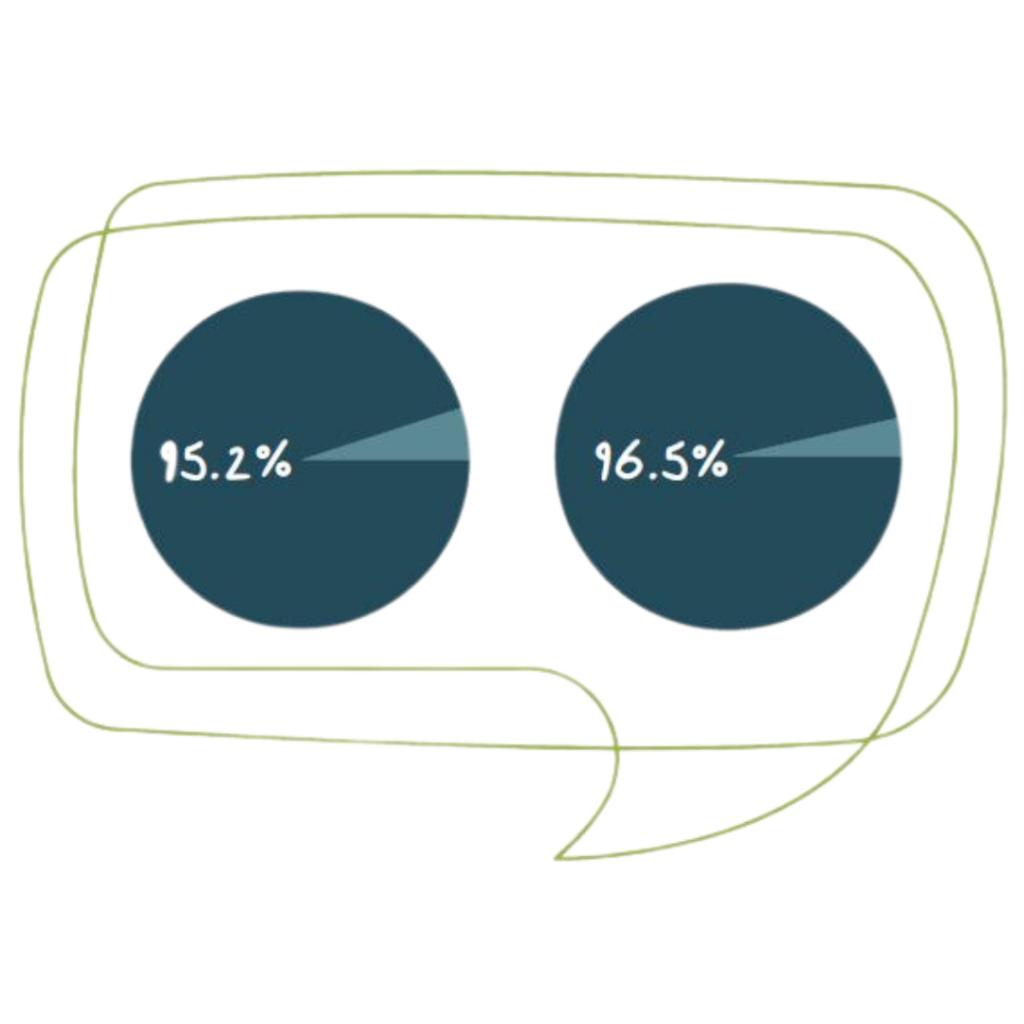
Complete Abstinence
At both 3 and 6 months following discharge, a substantial number of patients
with alcohol and other substance use disorders report maintaining complete abstinence.
To learn more about Ashley’s research programs, recent publications, and outcomes studies please contact us through the form below.
"*" indicates required fields